Hospitals and health systems across the country are reexamining their clinical service line strategies and operations in response to the shift from volume to value. In addition to population-based and episode-based payment reforms initiated by public and private payers, providers are challenged by mergers and acquisitions, clinical integration, consumerism and price transparency. Strengthening clinical service line strategies and capabilities are critical approaches to addressing these many challenges.
This post is the fourth in a four-part series where we introduce the pillars of success for clinical service lines: Governance and Leadership, Clinical Integration, Clinical Transformation, and Analytics and Innovation.
The Four Pillars of Clinical Service Line Success
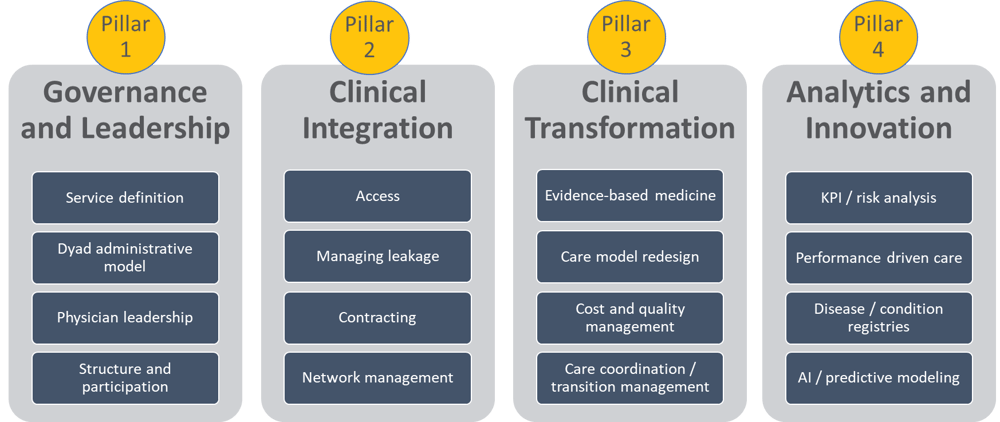
In this post, we address pillar four: Analytics and Innovation.
KPIs and Risk Analysis
For many organizations, the development and management of clinical programs will require some investment in clinical and performance data to support the required changes. Historically, data has been isolated in silos, such as imaging or surgery. Successful service line organizations need to cut across silos and create data tools that map the entire clinical experience for each patient.
This requires a comprehensive set of information covering all the services provided. To be accountable to stakeholders, the leadership team will need to define a set of key performance indicators (KPIs) that will help participants understand successes and gaps in the service line’s performance. These KPIs might include:
- Revenue
- Costs
- Margin, or revenue minus costs
- Volume by service
- Service level by access staff, or ability to take calls, respond to questions, and check patients in and out quickly
- Patient satisfaction
Analysis and visualization tools help turn data into actionable information. However, if the outputs are not intuitive or not focused on the problems at hand, physicians will not engage with these tools.
Critically important is to involve physicians in the choice of analysis and visualization options so they engage with the tools and use the information to improve care and reduce costs. This is especially vital when encouraging physicians and staff to make information available in the clinical workflow. Physician involvement in tool selection can help minimize distractions and optimize usability.
Performance-Driven Care
Bringing together and implementing the many changes described in the four pillars to optimize service line outcomes and succeed in value-based care represents a major cultural change for most service line organizations. This culture change can be captured by the term performance-driven care, which represents the vision for care delivery and measurement, including the specific goals and outcomes desired by the service line.
Many of the approaches outlined in the previous post in this series on clinical transformation are central to achieving the desired outcomes, especially the active engagement and participation of physicians throughout the change process.
The human and behavioral aspects of cultural change are the most important – as well as the most difficult. Along with engagement and participation, alignment of financial and intrinsic incentives for physicians and other clinical and managerial staff with the desired changes is a key lever in facilitating behavior change. Ensuring frequent and detailed communication from physician and administrative leaders regarding requirements for change is necessary. The communication needs to include the vision for future care delivery and the improvements to patient and provider experience. This kind of visioning exercise is key to facilitating behavior change.
Lastly, education and training to enable impacted leadership, clinicians, management, and staff to perform new work processes and job requirements are mandatory for success.
Disease and Condition Registries
Capturing clinical outcomes and utilization as a result of clinical variation efforts and the use of digitized care plans into shared longitudinal registries will create new population insights for specialty service lines.
Disease registries will also open new research and care model application opportunities that have yet to be imagined. These data-driven insights will enable service line providers to engage in a process of continuous improvement resulting in better and more efficient care.
Artificial Intelligence (AI) and Predictive Modeling
Digitizing care plans can help specialty providers implement treatment decisions and algorithms that have already been decided on, but the next question involves the role for machine learning to more deeply support health care decision making.
In the most basic of applications, artificial intelligence takes the form of monitor alerts in the ICU or drug interaction warnings in the EHR. This form of guidance will and should evolve to include background algorithms that suggest treatment pathways and provide likelihood of potential outcomes and risks. Ultimately, this will reduce care variation and drive the best quality and outcomes while managing service line patients.
That said, machine learning will not and should not replace or override human decision making in clinical care delivery. Too many situations exist that require the learning, practice, and experience of bedside caregivers. Even though computers are fast and accurate at analyzing data, complex and urgent situations still require experienced clinicians at all levels to make the best decisions.
In summary, clinical service lines prioritize analytics and innovation as the fourth pillar of success in value-based contracting. This includes KPIs and risk analysis, performance-driven care, disease and condition registries, and artificial intelligence and predictive modeling.
Please also read the three previous posts in this four-part series covering Governance and Leadership, Clinical Integration, and Clinical Transformation.



Share this: